Background: Device-associated health care-associated infections (DA-HAIs) in intensive care unit (ICU) patients constitute a major therapeutic issue complicating the regular hospitalisation process and having influence on patients’ condition, length of hospitalisation, mortality and therapy cost.
Methods: The study involved all patients treated > 48 h at ICU of the Medical University Teaching Hospital (Poland) from 1.01.2015 to 31.12.2017. The study showed the surveillance and prevention of DA-HAIs on International Nosocomial Infection Control Consortium (INICC) Surveillance Online System (ISOS) 3 online platform according to methodology of the INICC multidimensional approach (IMA).
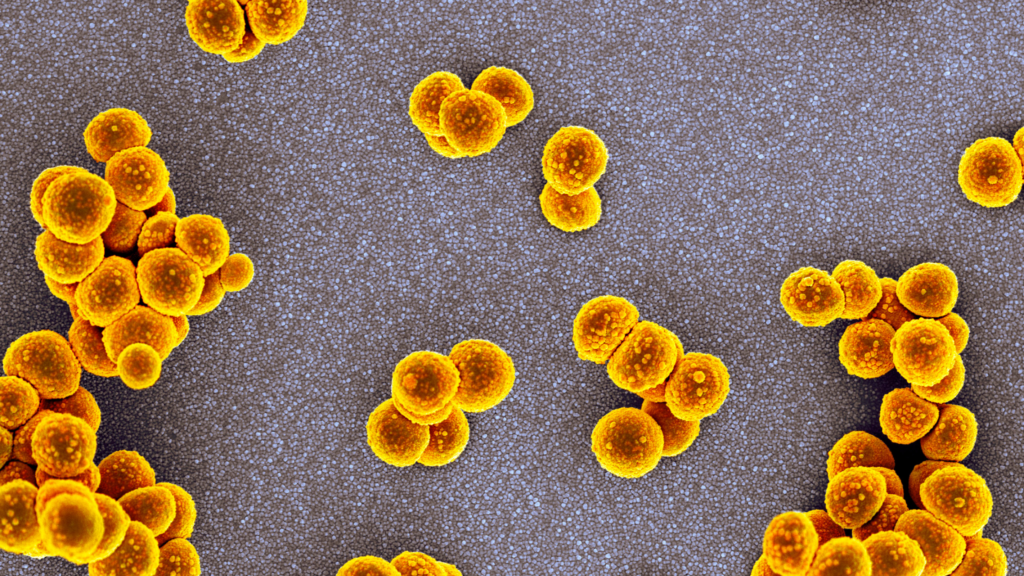
Results: During study period 252 HAIs were found in 1353 (549F/804M) patients and 14,700 patient-days of hospitalisation. The crude infections rate and incidence density of DA-HAIs was 18.69% and 17.49 ± 2.56 /1000 patient-days. Incidence density of ventilator-associated pneumonia (VAP), central line-associated bloodstream infection (CLA-BSI) and catheter-associated urinary tract infection (CA-UTI) per 1000 device-days were 12.63 ± 1.49, 1.83 ± 0.65 and 6.5 ± 1.2, respectively. VAP(137) constituted 54.4% of HAIs, whereas CA-UTI(91) 36%, CLA-BSI(24) 9.6%.The most common pathogens in VAP and CA-UTI was multidrug-resistant (MDR) Acinetobacter baumannii (57 and 31%), and methicillin-resistant Staphylococcus epidermidis (MRSE) in CLA-BSI (45%). MDR Gram negative bacteria (GNB) 159 were responsible for 63.09% of HAIs. The length of hospitalisation of patients with a single DA-HAI at ICU was 21(14-33) days, while without infections it was 6.0 (3-11) days; p = 0.0001. The mortality rates in the hospital-acquired infection group and no infection group were 26.1% vs 26.9%; p = 0.838; OR 0.9633;95% CI (0.6733-1.3782). Extra cost of therapy caused by one ICU acquired HAI was US$ 11,475/Euro 10,035. Hand hygiene standards compliance rate was 64.7%, while VAP, CLA-BSI bundles compliance ranges were 96.2-76.8 and 29-100, respectively.
Conclusions: DA-HAIs was diagnosed at nearly 1/5 of patients. They were more frequent than in European Centre Disease Control report (except for CLA-BSI), more frequent than the USA CDC report, yet less frequent than in limited-resource countries (except for CA-UTI). They prolonged the hospitalisation period at ICU and generated substantial additional costs of treatment with no influence on mortality. The Acinetobacter baumannii MDR infections were the most problematic therapeutic issue. DA-HAIs preventive methods compliance rate needs improvement.
References:
Duszynska, W., Rosenthal, V. D., Szczesny, A., Zajaczkowska, K., Fulek, M., & Tomaszewski, J. (2020). Device associated -health care associated infections monitoring, prevention and cost assessment at intensive care unit of University Hospital in Poland (2015-2017). BMC infectious diseases, 20(1), 761. https://doi.org/10.1186/s12879-020-05482-w